Drug addiction is a complex disorder. Addiction is characterized by compulsive drug-seeking and drug-taking that occurs even with the knowledge that these behaviors have severe adverse side effects. As a complex mental disorder, drug addiction likely involves altered biochemical signals that lead to dysfunction and the addictive behaviors. It is well documented that dopamine is an important neurochemical signal that is changed in drug abuse, however it is certainly not the only neurotransmitter signal that is changed.
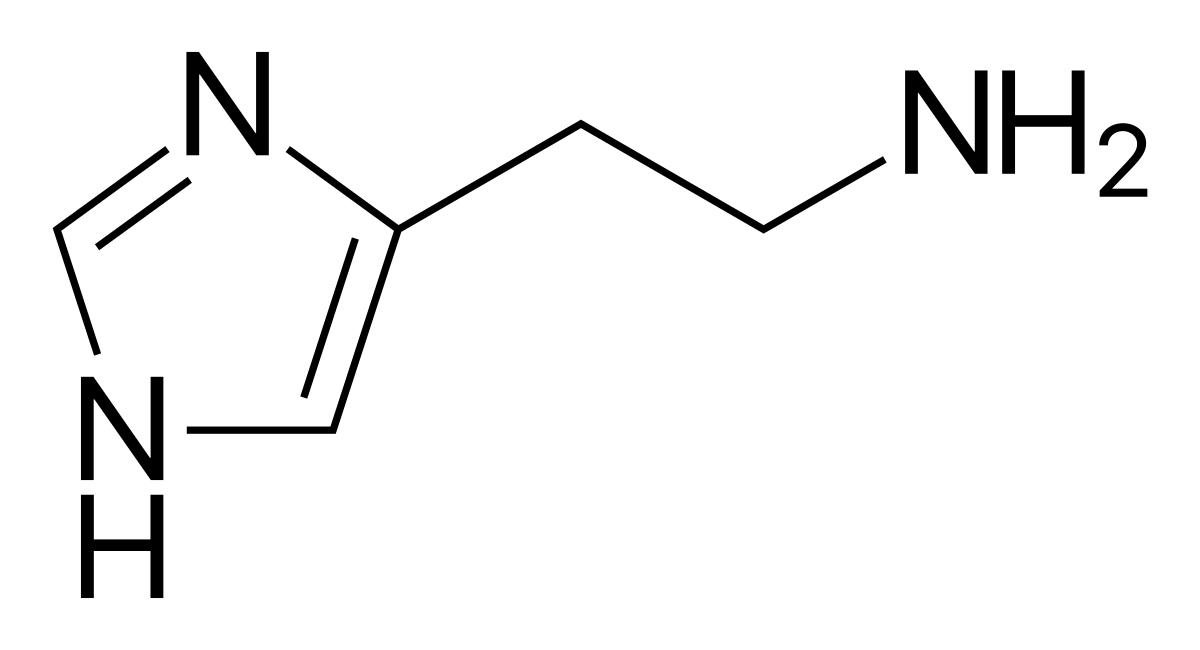
Histamine is believed to be dysregulated in drug abuse. Histamine is a neurotransmitter that is most known for its involvement with the sleep-wake cycle and the itch response. As a wake-promoting substance, when histamine receptors are blocked, a subject becomes sleeper - which explains when some antihistamine medications like benadryl (diphenhydramine) make us sleepy!
Anatomy of histamine neurons
Histamine is produced in the brain almost entirely by a small region of the brain in the hypothalamus called the tuberomammillary nucleus (TMN). Although small in volume, about 64,000 neurons in the human TMN, the TMN sends very diffuse histaminergic projections throughout several areas of the brain. Two regions of particular interest in the context of drug abuse and addiction are the striatum and the prefrontal cortex. Both of these structures receive histaminergic fibers as demonstrated with immunohistochemical analysis (Histamine-immunoreactive nerve fibers in the rat brain). Also, the TMN receives innervation from the infralimbic cortex.
Histamine in the striatum
The striatum is a brain structure that is important for integrating signals and determining an appropriate motor response. Almost all drugs of abuse involve some sort of physical behavioral component. For example, consider nicotine addiction via cigarette smoking. There is a very physical component that is involved with smoking, such as flicking the lighter, holding the cigarette, inhaling deeply, etc. Because there is a close connection between physical actions and the administration of nicotine, there is reason to believe that the striatum is dysregulated in drug abuse. Since histamine is released synaptically into the striatum, it may be possible to change the motor component of drug abuse by altering histaminergic tone.
Histamine in the prefrontal cortex
The prefrontal cortex (PFC for short) is a part of the frontal lobe that is responsible for higher order functions such as planning and volition. One of the signs of a chronic drug abuse problem is the continuation of drug use even despite the severe adverse consequences, such as financial troubles or detriment to personal health. Therefore, it would be reasonable to think that PFC function may be altered in people with substance misuse disorders, since these higher order planning behaviors seem deficient. Because histamine that is produced by the tuberomammillary nucleus is released into the PFC, it is possible to modulate the behavior of the PFC circuitry by synaptic release of histamine.
Infralimbic cortex control of histamine
The infralimbic cortex, a region of the medial prefrontal cortex, sends axonal projections into the TMN. Although the neurons of the TMN are usually tonically active, firing action potentials at a steady rate, their activity can be modulated by external signals. The infralimbic cortex therefore helps to regulate histaminergic tone in the brain.
Histamine receptors
Histamine acts as a natural agonist that can bind to and activate transmembrane receptors. In the human, we have so far identified for classes of histamine receptors.
H1 receptor
The H1 histamine receptor is a G-protein coupled with Gq. Activation of H1 receptors increase the activity of phospholipase C (PLC) which triggers the formation of two intracellular chemical signaling molecules, IP3 and DAG. The H1 receptor is expressed widely across the brain.
Nicotine addiction has been demonstrated to be sensitive to histaminergic H1 modulation. An experiment published in 2016 examined the role of chronic nicotine perfusion (similar to a nicotine patch) or chronic pyrilamine on intravenous self administration of nicotine. They discovered that the H1 antagonist pyrilamine decreased the rats’ desire to give themselves nicotine (Reduction of Nicotine Self-Administration by Chronic Nicotine Infusion with H1 Histamine Blockade in Female Rats). A related experiment conducted by the same group went on to study the effect of the H1 receptor antagonist pyrilamine on a nicotine self administration paradigm following an oral motor response. Specifically, the motor response examined is the operant licking of a waterspout that results in an automatic intravenous infusion of nicotine. Pyrilamine given via a subcutaneous injection, led to a decrease in licking behavior, resulting in decreased self administration of nicotine (IV Nicotine Self-Administration in Rats Using a Consummatory Operant Licking Response: Sensitivity to Serotonergic, Glutaminergic and Histaminergic Drugs). Collectively, these two studies indicate that decreasing histamine H1 activation may be useful in helping decrease nicotine addiction.
Histamine H1 antagonists may be difficult to use clinically, since H1 antagonists may cause a person to become very sleepy.
H2 histamine receptor
The H2 receptor is a G-protein coupled with Gs. Activation of this receptor results in increased cellular excitation through an increase in adenylyl cyclase, an enzyme that synthesizes cyclic AMP (cAMP). This can then trigger activity of protein kinase A, which excites the cell.
Tone of the H2 receptor is modulated by chronic exposure to methamphetamine. In one experiment by the Watanabe lab in Japan published in Neuroscience Letters in 1999, they looked at mRNA levels of the histamine H2 receptor after giving rats methamphetamine chronically for 21 days. In their hands, it was found that the mRNA for the H2 receptors were elevated only at the time point of seven days after discontinuation of methamphetamine. However, there was no significant elevation of the H2 receptor mRNA at 1 day of withdrawal or 14 days withdrawal. In their interpretation of the data, they conclude that methamphetamine withdrawal may be mediated in part by the histamine H2 receptor at a one week withdrawal point, but not significantly immediately after withdrawal (Transient increases of histamine H1 and H2 receptor mRNA levels in the rat striatum after the chronic administration of methamphetamine)
H3 histamine receptor
The H3 receptor is a G-protein coupled receptor that is linked with Gi/o proteins. Binding of an agonist to the H3 receptor leads to cellular inhibition by the decrease of adenylyl cyclase activity, thereby decreasing both cAMP and PKA activity.
Histamine H3 receptor antagonists are involved in ethanol mediated behavior. One study tested the novel H3 receptor antagonist called DL77 on a two-bottle choice paradigm in mice. In this behavioral test, the mouse is presented with two different bottles, one of which contained alcohol while the other was normal water. During the test, blockade of the H3 receptors led to decreased alcohol seeking, and less alcohol consumption. (The novel non-imidazole histamine H3 receptor antagonist DL77 reduces voluntary alcohol intake and ethanol-induced conditioned place preference in mice.)
H4 histamine receptor
The H4 receptor, like the H3 receptor, is a Gi/o coupled inhibitory metabotropic receptor. However, it is not heavily expressed in the brain. Most of the H4 receptor is outside of the central nervous system, with strong expression in the liver, gut, and blood.